Article Type: Products
Naked Prosthetics
Naked Prosthetics designs and fabricates durable, custom prosthetic devices specifically for those living with finger loss.
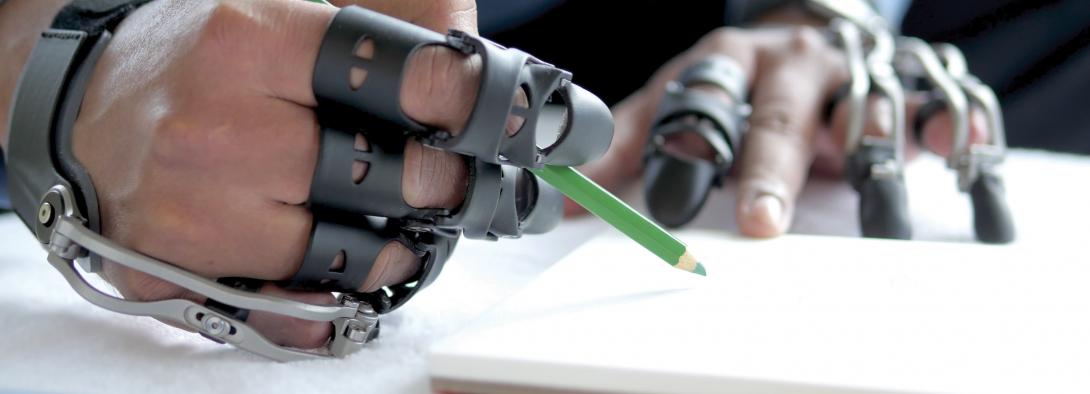
“Our mission is to assist people with finger amputation and to positively impact their lives by providing functional, high-quality finger prostheses.” With a range of options for varying degrees of finger loss, Naked Prosthetics finger prostheses continue to enable amputees to live active and independent lifestyles.
Product Range
| PIPDriver™ | |
| Designed for individuals amputated at the middle phalanx. The PIPDriver™ is the most simple and intuitive to use. Because the device fits alongside the patient’s finger, we can anatomically match their PIP and DIP joints so it operates predictably and naturally. The PIPDriver™ offers exceptional daily utility. The second-generation PIPDriver™ combines the same reliable functionality with a new, sleek aesthetic design, improved hinges, and a variety of colour options for users. |  |
|
|
|
| ThumbDriver™ | |
| The newest product in our lineup shares its heritage with the MCPDriver™. It features a unique anchor design that tracks the patient’s natural CMC motion while still providing a rigid structure to react to the heavy forces generated by thumb opposition. The tip is positionable and articulates more subtly than in the MCPDriver™, which enables the most common thumb grasps. |  |
|
|
|
| MCPDriver™ | |
| Designed for amputations at the proximal phalanx, the MCPDriver™ restores the middle and distal phalanges. These dependently articulating pads help to create natural grip patterns. (The MCPDriver™ excels at restoring pinch, key, and cylindrical grasps as well as grip stability.) The durable metal frame and replaceable components allow users to return to particularly demanding lifestyles with confidence. The second-generation MCPDriver™ features improved aesthetic appearance and comfort, precision-machined components, and stylish colour options. |  |
|
|
|
| GripLock Finger™ *NEW* | |
| The GripLock Finger™ is Naked Prosthetics’ elegant solution for amputations proximal to the MCP joint. This device can be worn in conjunction with our MCPDriver™, PIPDriver™ or ThumbDriver™, and provides the same colours and design choices our users love. Serviceable nylon fairings and silicone pads provide seamless aesthetics and improved grip stability while also preventing scratch damage to sensitive surfaces and objects handled by the user. |  |

oapl have a vast array of experience treating patients with finger amputation.
To book an appointment with one of our prosthetists, please call us on 1300 866 275 or view our clinical locations here.